#What is ETC02?
End tidal C02 is the measurement of the partial pressure of C02 gas which is expired during exhalation. The measurement is taken at the end of exhalation in an attempt to measure when the exhaled gas will most likely match the alveolar C02 concentration.
Capnometry was first used in World War II to measure atmospheric C02 levels. Its first use in medicine was in 1950 to measure exhaled C02 in anaesthetised patients. Capnometry had a more widespread adoption in the 1980’s with the development and production of smaller capnometry machines.
The measurement of ETC02 has two parts, the numerical measurement (Capnometry) and the waveform (Capnography). A thorough understanding of both is important.
Metabolic, perfusion, and ventilation status can be reflected in real time through the measurement of ETC02. Highlighting the importance of its use in critically unwell patients.
#The science behind ETC02
C02 is a byproduct of cellular metabolism. Put simply, Cells take in Oxygen and glucose, and create carbon dioxide (C02), water and energy (ATP). C02 is then bound to haemoglobin via as series of reactions and carried via the blood stream to the lungs, where removal from the body occurs through gas exchange with the atmosphere.
CO2 plays an important role in acid-base balance.
The equation below represents Bicarbonate-Carbonic acid buffer system:
C02 + H20 <—> H2C03 <—> H + + HC03-
When C02 levels are high, there is a rightwards shift of the reaction. This results in an increased amount of H+ ions released into the bloodstream, lowering blood pH subsequently resulting in acidosis.
How does C02 exchange work in the lungs?
Well, gas exchanges occur through gas diffusion. Gasses diffuse from areas of higher concentration to areas of lower concentration, following a concentration gradient. In the pulmonary artery, deoxygenated blood has a partial pressure of carbon dioxide (pc02) of approximately 46 mmHg and a partial pressure of oxygen (P02) is roughly 40 mmHg. This results in Oxygen from the alveolus (p02 of ~100 mmHg) to diffuse into the pulmonary artery, and C02 to diffuse into the alveolus (pc02 of ~40mmHg) and be expelled into the atmosphere. This is where etc02 measurement occurs.
#What is dead space? Does it matter?
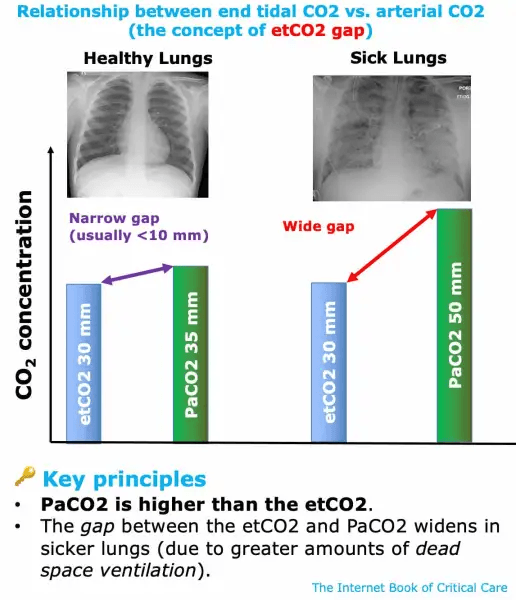
When talking about ETC02, dead space refers to inhaled gases that do not participate in gas exchange. The etc02 measurement is usually 2-5 mmHg lower in etc02 than pac02 - although this can be significantly effected in certain conditions. This can happen for 3 reasons:
- Anatomical dead space
- Trachea and large bronchi - Gases in these spaces do not participate in gas exchange.
- Instrument dead space
- Breathing circuits, ET tube, Igel
- Alveolar dead space
- Dysfunctional alveoli which receive ventilation but don’t exchange C02. This is most notable in patients with diseased lungs.
What is the correlation between dead space and etc02? Well, simply put, with increasing dead space, especially alveolar or physiological dead space, will represent a difference between etc02 measurements and pac02.
For example, alveolar dead space may be increased in a patient with a lung dysfunction at the alveolar, vascular or airway level. Pulmonary embolism, pneumonia, aspiration and asthma are all examples of conditions which can significantly increase alveolar or physiological dead space.
credit EMcrit
Dead space is a concept used to theorise the difference between etc02 and Pac02. Increased dead space can lead to low etc02 levels, although this is something we can not measure in the prehospital setting.
Can the theory of dead space be applied in the prehospital setting? Maybe. For example, you have a patient who you suspect has a pulmonary embolism, this would create a alveolar dead space. Some studies suggest an etc02 >35 mmHg can almost rule out a PE with a negative predictive value of 95% —> 100%. 1, 2, 3
#Cardiac output and ETC02
Does cardiac output affect ETC02? Well, transiently.
For example, lets think about etc02 during cardiac arrest. You may have initially low ETC02 levels due to no cardiac output. High quality CPR will drastically increase cardiac output and increase the etc02. If ROSC occurs, then a spike in etc02 may occur.
Another example is during a leg raise during hypotension. This will temporarily increase cardiac output and is a good predictor of patients who will be preload-responsive. If increase in cardiac output occurs, a transient increase in etc02 will occur.
#Mainstream or Sidestream ETC02 monitoring
Mainstream ETC02 monitors sit directly above the airway adjunct, inline with the airway circuit. An example of this is the EMMA device. This allows for the expired gass to pass the infrared light path and results in almost immediate reading of ETC02. This allows for fast response times. The main disadvantage of a mainstream device is its difficult/impossible use on spontaneously breathing patients.
Sidestream ETC02 monitors sit away from the airway circuit. The ETC02 monitoring on the corpuls is a sidestream device. Sidestream monitors take samples of the expired gas through an adjunct in the airway circuit. The corpuls achieves this through the use of a pump. Sidestream devices enable versatility in measurement through a variety of measurement devices, like nasal prongs and circuit attachments.
Mainstream and sidestream devices provide quantitative data, as they provide a numerical value for ETC02.
Colourmetric devices are a qualitative device which provides a range of values represented by colours. These devices can be termed C02 detectors, and not monitors. Historically, they were used within ambulance to ensure the presence of C02 post intubation. Colourmetric devices are considered mainstream devices, although their use is as a last resort, if all other devices fail.
#ETC02 measurements and waveforms
Assessment of ETC02 is multifaceted. During ETC02 monitoring you receive capnography and a capnometry.
Capnometry measures ETC02 through numerical representation only, where as Capnography is inclusive of numerical measurement and displays a waveform.
Another crucial aspect of ETC02 monitoring is the Capnograph. The capnograph represents a inspiratory, expiratory waveform.
Many factors can effect the ETC02 reading and waveform. Below is a graph of common waveforms.
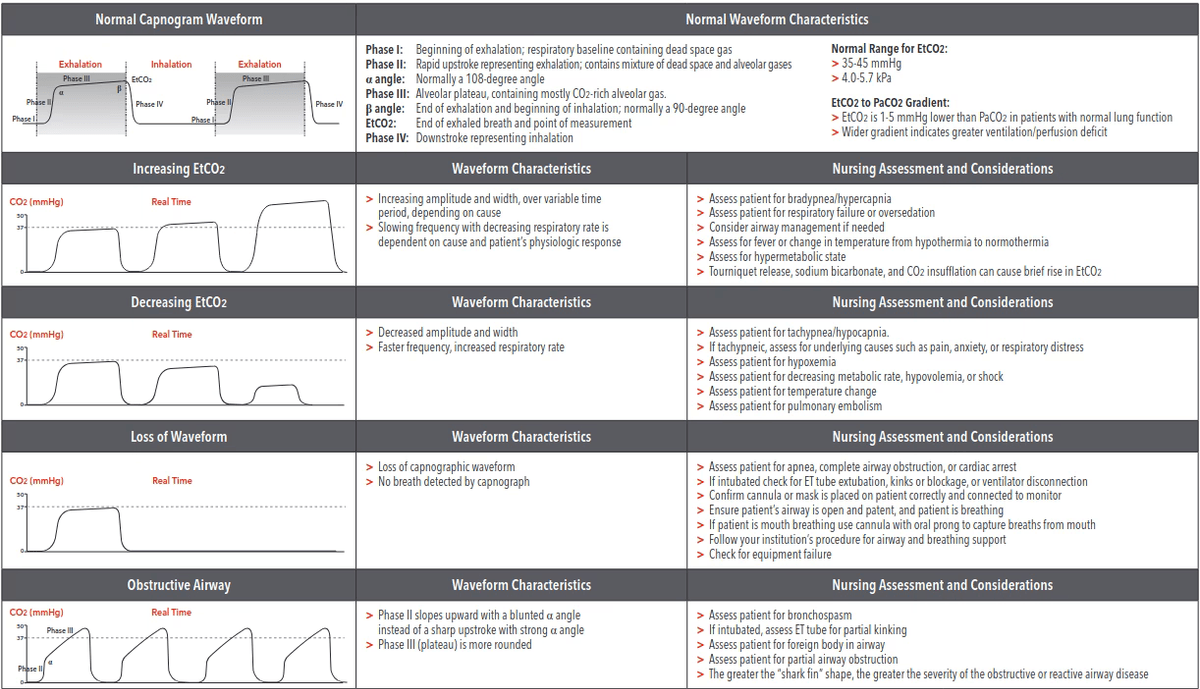
Some factors that can effect ETC02 readings:
Low ETC02
| Failure of ventilation | Circulatory failure | Increase RV afterload | Other |
|---|---|---|---|
| Circuit disconnection | Cardiac arrest | PE | Hyperventialtion |
| Airway obstruction | Worsening shock | High PEEP | |
| Bronchospasm | Reduced cardiac output | ||
High ETC02
| Decreased ventilation | Increased C02 production | Increased inspired C02 |
|---|---|---|
| Decreased RR | Sepsis | Rebreathing |
| Decreased Tidal volume | Tourniquet release | External C02 source |
| ROSC | ||
| Malignant hyperthermia | ||
#Who should receive ETC02 monitoring? How can it help?
ETC02 can be a useful tool in many scenarios. It provides useful, realtime feedback about a patients respiratory function and status. etco2 is a useful and necessary adjunct to confirming ETT placement.
Patients who should receive ETC02 monitoring is up to the discretion of the provider.
A short list of patients who could benefit from ETC02:
| Parental sedation | Respiratory | Trauma | Low perfusion states |
|---|---|---|---|
| Droperidol | Asthma | Head injuries | DKA |
| Midazolam | COPD | Chest injuries | Sepsis |
| Morph/Midaz | APO | Multi-system trauma | Cardiogenic Shock |
The table above demonstrates a small cohort of patients who could benefit from ETC02 monitoring.
Can you think of any other patients who could benefit from ETC02 monitoring?
End tidal can be a useful adjunct to treatment. It allows the provider to have another tool to assess respiratory/ventilatory/circulatory status. It is important to understand how to interpret and diagnose reasons for low and high etc02 readings.
Here is a short video from LITFL on the use of ETC02 in cardiac arrest
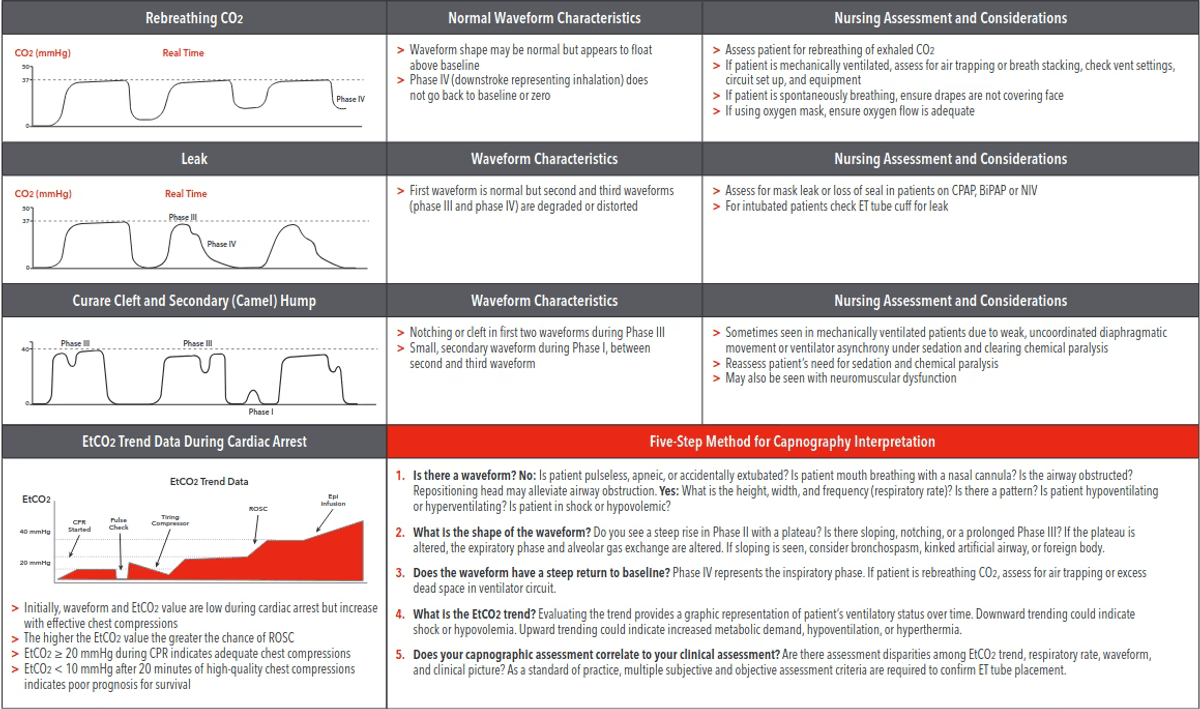
ETC02 can prove as a beneficial assessment of CPR quality. ETC02 should rise to near normal levels or >30 mmHg with good CPR. Fatigue will show immediate decrease in ETC02 and should be an indicator to swap CPR providers. Inversely, a sharp rise in ETC02 can be an indicator of ROSC. A sharp rise in ETC02 to normal or above normal levels indicates cardiac output.
An ETC02 of <10 mmHG or equal to 10 mmHg after 20 mins of ACLS has a positive predictive value of 100% of mortality. Persistently low ETC02 during CPR in intubated patients suggests ROSC is unlikely. ETC02 levels near normal for cardiac arrests up to 60 minutes have show survival to discharge rates of almost 20% in persistent VT/VF arrests.
ETC02 monitoring can prove useful in the prevention of hyperventilation of patients during post ROSC care. Aim for a ETC02 of 35-45 mmHg.
Most studies have show the usefulness of ETC02 levels after 20 mins of CPR:
- etc02 <10 mmHg suggest low likelihood of survival (asystole and etc02 <10 suggest futility)
- etc02 10-20 mmHg is a grey zone
- etc02 >20 mmHg suggest a higher likelihood of survival
etc02 levels are a guide, with other factors taken into account in the context of cardiac arrest.
The use of ETC02 in respiratory patients can show efficacy of treatment or be a predictor of deterioration. To note, ETC02 during respiratory/cardiac arrest due to asthma/COPD ETC02 levels can be extremely high (80-100 mmHg). Trying to lower ETC02 in this cohort of patients is not advised, as poorer outcomes are likely. ETC02 can be a guide to efficacy of drug therapies.
Use in trauma and head injury can be beneficial. For example, patients with chest/head trauma. Chest injuries can lead to tension pneumothorax and head injuries can have a direct effect on respiratory status. ETC02 can play a role in respiratory/airway management and monitoring in these patients.
Use in a range of patients presenting with metabolic disorders can prove useful. Take for example, you have a patient you suspect has DKA. They’re hyperglycemic, present with abdominal pain, nausea, vomiting. ETC02 can be a useful tool to help affirm diagnosis. Literature suggests that an ETC02 >26 mmHg can effectively rule out the presence of DKA.
Capnography can be used to estimate shock intensity. ETC02 will be lower in patients in a significantly volume-shocked stated. This is due to reduced cardiac output, and less flow through the pulmonary circuit. A reduction in pulmonary gas exchange occurs and a reduction in ETC02 occurs. ETC02 can prove to be a useful tool to help evaluate success of treatment and severity of shocked patients.
ETC02 can prove to be a useful adjunct in many scenarios. It provides direct and almost instantaneous feedback to the provider. It can be a great indicator of how well your treatment is working, and an early sign of changes in a patients respiratory/haemodynamic/metabolic status if used appropriately and well. Hopefully you will feel more comfortable using ETC02 as an adjunct to your treatment.
#References
- EMCrit - C02
- End tidal carbon dioxide monitoring in prehospital and retrieval medicine: a review
- American Nurse - Understanding end-tidal CO2 monitoring
- Acid-Base Balance - Oregon State University
- Physiology, Carbon Dioxide Retention
- End-Tidal and Arterial Carbon Dioxide Measurements Correlate Across All Levels of Physiologic Dead Space
- Estimating Arterial Partial Pressure of Carbon Dioxide in Ventilated Patients: How Valid Are Surrogate Measures?
- The combined use of end-tidal carbon dioxide and alveolar dead space fraction values in the diagnosis of pulmonary embolism
- The combined use of end-tidal carbon dioxide and alveolar dead space fraction values in the diagnosis of pulmonary embolism
- End-tidal CO2 for exclusion of suspected pulmonary embolism: a new partner for Wells?
- Is Bedside End-Tidal CO2 Measurement a Screening Tool to Exclude Pulmonary Embolism in Emergency Department?
- ETCO₂: a predictive tool for excluding metabolic disturbances in nonintubated patients
- Applications of End-Tidal Carbon Dioxide (ETCO2) Monitoring in Emergency Department; a Narrative Review
- Capnography as a tool for triaging and diagnosis of diabetic ketoacidosis in the emergency department: A prospective observational study