#Preface
While isolated beta-blocker overdoses are generally considered less severe, certain beta-blockers can exhibit profoundly toxic effects. For instance, propranolol can cause significant sodium channel blockade, akin to tricyclic antidepressants (TCAs), while sotalol is known for its potassium channel blockade, which can result in a prolonged QT interval and a heightened risk of Torsades de Pointes (TdP).
#Mechanism
Beta-blockers function by competitively binding to beta-1 and beta-2 adrenergic receptors located in various systems, including the cardiovascular system, lungs, eyes, and liver. By binding to these receptors, beta-blockers reduce the production of intracellular cyclic adenosine monophosphate (cAMP), which diminishes the effects of catecholamines (such as adrenaline and noradrenaline). This reduction in cAMP leads to decreased heart rate, blood pressure, cardiac contractility, and blood sugar levels.
In cases of overdose, beta-blockers can cause cardiovascular shock. This may force the cardiovascular system to rely more on glucose rather than fatty acids, which can result in decreased ATP production. Propranolol, a non-selective beta-blocker, can also cause sodium channel blockade, while sotalol, another non-selective beta-blocker, additionally inhibits potassium channels. This can lead to a prolonged QT interval and an increased risk of TdP.
Beta-2 receptor blockade in the liver impairs glycogenolysis, gluconeogenesis, and lipolysis. While these effects are generally minimal under normal use, they can cause significant hypoglycaemia in diabetic patients, particularly in paediatric populations. During an overdose, hypoglycaemia can be profound.
Additionally, beta-2 receptor blockade in the peripheral vasculature and bronchial smooth muscle reduces the effects of catecholamines on smooth muscle contraction. This leads to peripheral vasodilation and can increase bronchial smooth muscle constriction, complicating the management of asthma and other related disorders due to reduced responsiveness to beta-2 agonists.
#Toxicokinetics
Beta-blockers are generally rapidly absorbed, reaching peak serum concentrations within 1-3 hours. Propranolol is highly lipophilic, meaning it is extensively distributed into fatty tissues and crosses the blood-brain barrier easily. In cases of overdose, the high lipophilicity of propranolol can lead to prolonged retention and extended elimination half-life. Additionally, because propranolol crosses the blood-brain barrier, it has significant central nervous system (CNS) effects, which is particularly important in cases of propranolol toxicity.
Beta-blockers like Propranolol are highly protein bound. For example, Propranolol is 90-95% protein bound. The high protein binding of beta-blockers has significant implications for drug toxicity. Since a large portion of the drug is bound to plasma proteins, only the free (unbound) drug is pharmacologically active and able to cross cell membranes. In cases of overdose, the proportion of free drug can increase if the protein binding sites are saturated or displaced by other substances. This can lead to higher concentrations of the free drug in the bloodstream and tissues, including the central nervous system. As a result, the risk of toxicity may be heightened, with potentially severe adverse effects. Moreover, in conditions that affect protein levels or function, such as liver or kidney disease, the drug’s distribution and elimination can be altered, further complicating the management of overdose and toxicity
#Clinical presentation
- cardiovascular effects
- hypotension due to a combination of myocardial depression and bradycardia
- sinus bradycardia (most common arrhythmia)
- first- to third-degree heart block, junctional bradycardia; ventricular bradycardia and asystole in severe poisoning
- QRS widening in propranolol poisoning
- QT-interval prolongation in sotalol poisoning
- central nervous system effects → seizures, delirium and coma if poisoning is due to a lipophilic beta blocker (eg propranolol)
- respiratory effects → bronchospasm and pulmonary oedema, especially in patients with airway disease
- metabolic effects → hypoglycaemia (uncommon) or hyperglycaemia.
#Video
#Propranolol
Class II antiarrhythmic. Nonselective beta-adrenergic blocker. Blocks both beta-1 and beta-2. Decreases heart rate, myocardial contractility, blood pressure, and myocardial oxygen demand.
#Preparations
- Commonly prescribed at dosages of 10mg-40mg in quantities of 100.
- Often taken 2-3 times daily to achieve maintenance levels of 120mg-320mg daily
#Overdose
2g is likely to cause significant toxicity although doses as low as 1g may cause severe toxicity usually with onset <6hrs
Toxicity will manifest within 4hrs unless extended release preparation is ingested.
- Bradycardia
- Hypotension
- Sodium channel blockade (QRS Widening)
- Seizure, coma, and delirium
- CNS Depression
- Bronchospasm
- HyperK+
- Hypoglycaemia
#Prehospital treatment
Prehospital treatment is limited and usually requires advanced clinical interventions. Initial management includes:
- Treating hypotension with 20 ml/kg of Hartmann’s solution.
- Adrenaline infusion and/or transcutaneous pacing.
- Ensuring rapid airway management
- Correcting hypoxia is crucial. Acidosis significantly exacerbate sodium channel toxicity.
Sodium Bicarbonate:
- Administer 1 mmol/kg (maximum 100 mmol bolus) to address sodium channel blockade. Due to the limited initial dose, repeat doses may be necessary. Consultation with ACCC/Poisons is recommended for guidance on dosing.
Contraindications:
- Amiodarone is contraindicated in the treatment of propranolol overdose.
Rapid treatment and transport is essential in cases of significant overdose. In-hospital treatment involves intensive care, including insulin/glucose therapy for increased inotropy, specific vasopressor therapy, and possibly trans venous pacing (with transcutaneous pacing often being ineffective).
#PEARLS
- High Lipophilicity (Increased CNS effects)
- Rapidly crosses blood-brain barrier (Seizure, CNS depression, delirium)
- sodium channel blockade
- hyperK+
- hypoglycaemia
#ECG
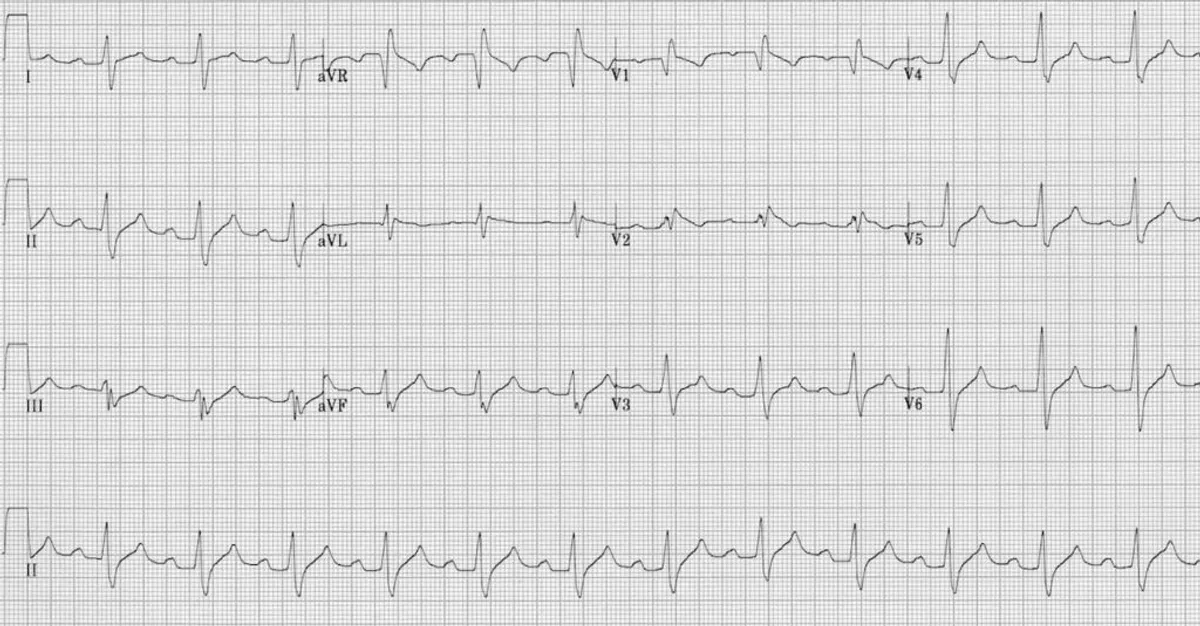
ECG demonstrating the key features of Propranolol overdose
Note: This is an ECG of flecainide toxicity - Propranolol will have a slower HR.
- Positive R wave in AVR
- Wide QRS (>100ms)
- 1st degree AV block
#Sotalol
Class III antiarrhythmic and non-selective beta-adrenergic receptor blocker. At therapeutic doses, it primarily exhibits beta-blocking effects. However, at doses exceeding 160 mg/day, sotalol also affects cardiac potassium channels, prolonging the QTc interval and significantly increasing the risk of TdP and other ventricular dysrhythmias.
#Preparations
- Available in 80 mg and 160 mg oral tablets, typically in packets of 60
#Brand names
- Betaloc
- Locasol
- Sitaglo
- Sotacor
- Sotalol Sandoz
#Overdose
In overdose, sotalol exhibits potent beta-1 and beta-2 adrenergic receptor blocking effects, which, in conjunction with its class III antiarrhythmic properties (Potassium channel blockade), can lead to significant prolongation of the QTc interval. This prolongation increases the risk of developing TdP, a potentially life-threatening ventricular arrhythmia characterized by a rapid, irregular heartbeat that can lead to sudden cardiac death if not promptly treated. The risk is particularly pronounced in patients with underlying conditions that predispose them to QTc prolongation or electrolyte imbalances, such as hypokalaemia or hypomagnesemia.
#Prehospital treatment
Bradycardia
- Atropine
- Adrenaline infusion
- Transcutaneous pacing
Hypotension
- fluid resuscitation - 20ml/kg bolus
- Adrenaline infusion
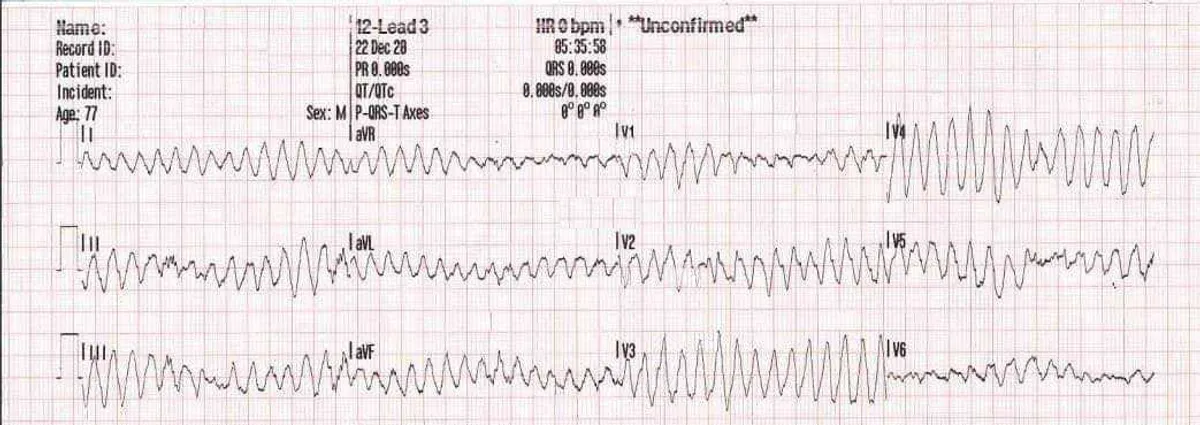
#Torsades de Pointes
The gold standard treatment for TdP is the administration of Magnesium Sulphate. In prehospital care, defibrillation is recommended for all patients who experience cardiac arrest due to TdP. Establishing venous access and applying defibrillation pads are essential for all patients suspected of a sotalol overdose, as these measures facilitate rapid intervention and potential stabilization.. Sotalol is dialyzable and in some cases ECMO can be extremely beneficial. Early access to intensivist and expert toxicological intervention is essential.
#PEARLS
- Bradycardia
- Hypotension
- Prolonged PR interval and Prolonged QTc >500ms
- Increased risk of TdP!
- Hypoglycaemia
#ECG
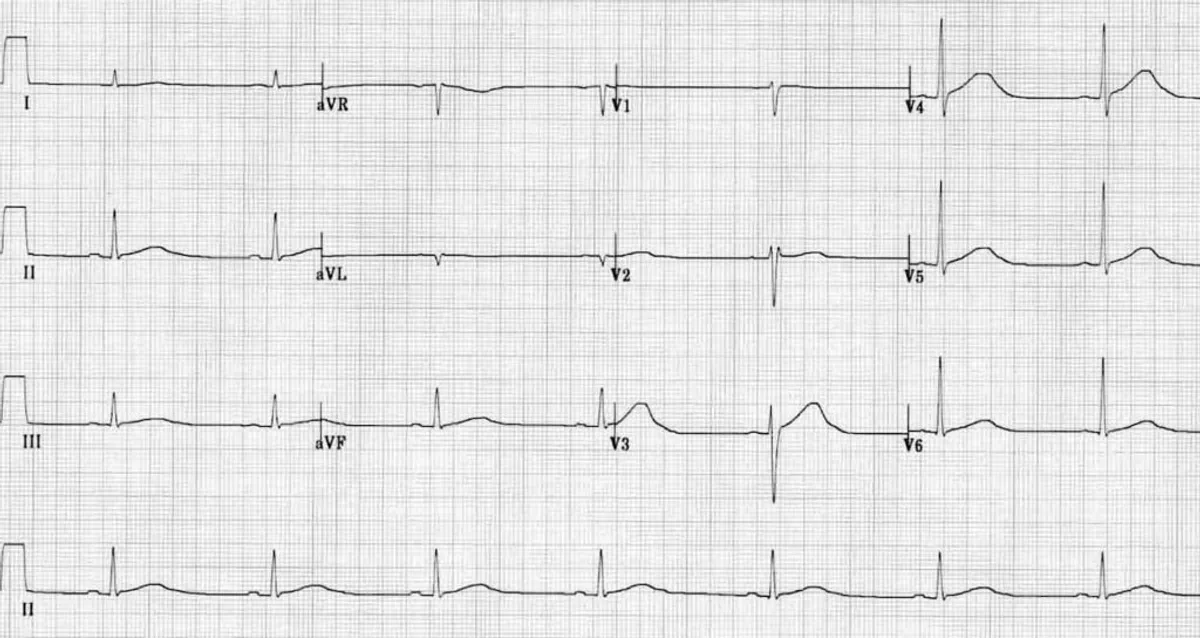
ECG from sotalol overdose
- Sinus bradycardia
- Severe QTc Prolongation (Roughly 600ms)
This patient is at significant risk of TdP!!!
#Some controversy
#Glucagon
Glucagon, was once widely recommended by toxicological societies as an adjunct for the treatment of beta blocker overdose. Glucagon works by increasing intracellular cyclic AMP, which enhances cardiac contractility and heart rate, counteracting the effects of beta-blockade. However, if the beta-blockade is profound, glucagon may not provide sufficient therapeutic benefit on its own. Anecdotally, not all patients respond adequately to glucagon. Little evidence supported treatment with glucagon. 1. Further, the dose of glucagon which was previously needed is significant. The recommended dose is in the range of 5-10mg IV, something that is rarely readily available. Glucagon has a stimulatory effect on the gastrointestinal tract Glucagon commonly induces vomiting significantly increasing aspiration risk! High dose Insulin euglycemic therapy is used in conjunction with fluid therapy and inotropes.
NSWA no longer recommends the use of Glucagon in bradycardia.
There have been no controlled trials to prove the efficacy of glucagon in poisoning beta-blocker overdose, glucagon can be considered as a useful treatment of choice6 although is not recommended by Australia Toxicology societies. Logistically, Glucagon can be difficult due to the large dose required, Risk of aspiration and anecdotal evidence of efficacy.
Read more Here
#Conclusion
Beta blocker overdose is potentially life threatening. The mainstays of treatment in the prehospital setting remain symptomatic. Treat aggressively and rapidly. Crystalloids and inotropy are key. Consideration of transcutaneous pacing, Rapid treatment of arrhythmias and rapid transport are essential.
#References
- Does glucagon really work?
- Beta-blocker overdose - LITFL
- Beta-blocker poisoning - Up To Date
- Beta-blocker poisoning - Therapeutic guidelines
- Sotalol ECG - LITFL
- Beta-Blocker Toxicity

